For Hepatitis Awareness Month, NVHR is going Back to Basics to raise awareness of hepatitis A, hepatitis B, hepatitis C, and hepatitis D.
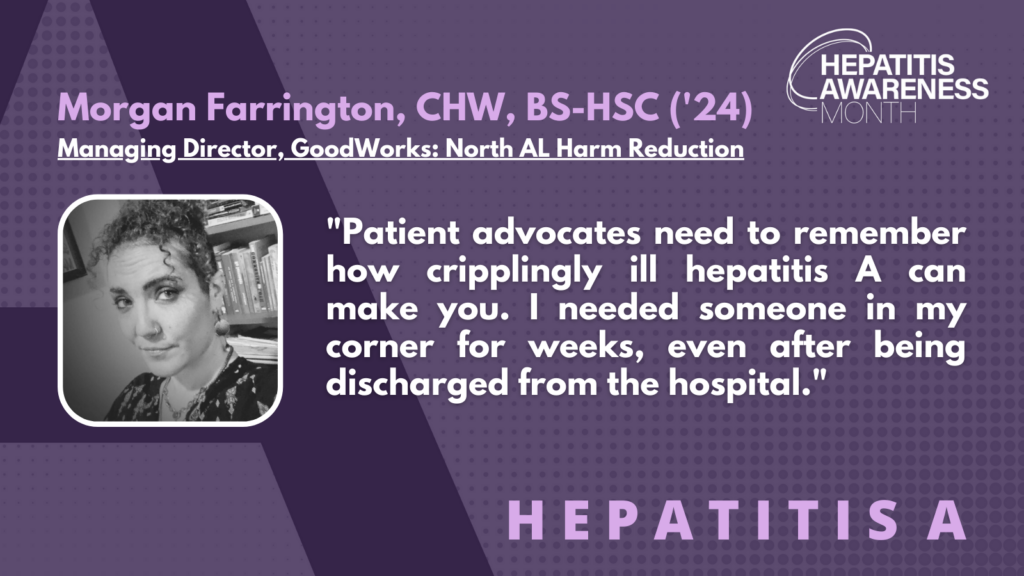
Morgan Farrington, CHW, BS-HSC (’24) (they/them), is the Managing Director of GoodWorks: North AL Harm Reduction and Robin Lord Smith is the Community Engagement Coordinator at National Viral Hepatitis Roundtable (NVHR). This interview has been lightly edited for clarity and length.
NVHR: What would you like to share with us about your journey with hepatitis A?
MF: I feel like it is not over yet. I had no idea how sick I was until I was pretty much on the floor unable to move. I wish that was an overstatement. I felt like it was possible that my stress and exhaustion level at that time had something to do with it, or that I was sick for a long time and had no idea. I was not paying attention to my body and was writing everything off as being tired and everything being hard. It was definitely a lesson learned to listen to my body.
NVHR: We’ve made progress in raising awareness about hepatitis A but work still remains. What are some of the most effective ways to raise awareness in your view?
MF: Smaller grassroot campaigns are effective. There are a lot of people who are at risk because of their lifestyle and the best way to reach them is through other members of their community. Hepatitis A has a high prevalence in communities of unhoused people so it can be difficult to get the word out. Our local jail has tremendous rates of infection and nothing is being done about it. Public awareness is how we can drive systemic change.
I also think that homeless encampments without clean running water needs to be addressed. The challenge is that the public does not see it as a risk they are subjected to, but it is a risk. In tight packed cities, when people get sick, they are easily spreading germs from one person to another. That’s why expanding people’s understanding of risk and their perception of personal risk is so important. We need to expand the idea of what personal responsibility means when it comes to public health.
NVHR: Do you have any priority actions as a hepatitis patient and advocate? What do you think is most needed for the community?
MF: We need to address some of the basic needs of people who are at higher risk for contracting hepatitis and be there for them. This includes providing access to clean running water, shelter, and healthcare. Alabama has not expanded Medicaid services, so if I were to choose to get insurance, it would cost more than my rent. If people have other health conditions, they are going to deteriorate faster. It’s also everyone’s responsibility to consider the health of those around you. If you are sick, stay home or go get treatment. Be conscious of the fact that just because something might not hurt you, it can kill someone else.
NVHR: What’s one thing you wish you knew when you started your hepatitis A journey?
MF: I wish I had thought about hepatitis A as a threat to my personal health more. I was thinking about hepatitis B, hepatitis C, HIV, and COVID-19 considering the recent increase in outbreaks in the community. The community that I move around in and work with are hyperaware of hepatitis C, but nobody really thinks about hepatitis A and how easy it is to pass around. One person told me they are sure they got infected because they took a bite off someone’s burger – something that seems completely harmless.
NVHR: What message would you like to share with other patient advocates about hepatitis A?
MF: Patient advocates need to remember how cripplingly ill hepatitis A can make you. I needed someone in my corner for weeks, even after being discharged from the hospital. I was in the middle of moving housing when it happened. I had to enlist help to move my entire house because I couldn’t do it myself. I felt helpless. I could not go back into the world by myself for at least two months. There are still days where I just kind of feel weird. It’s been three months now where I haven’t had to constantly worry about what I’m eating. If I had gone a few more days without medical attention after my first symptoms, I could have died. And I’m a person with access to food, water, a place to rest adequately, and a support system. A lot of people don’t have access to those resources and support and that’s why it’s so important that we are there for them.